Dizziness and Vertigo
Common ED presentation and one almost universally hated by EM clinicians, there is a suggestion that we misdiagnose up to 81% of vertigo patients. The first step in seeing these patients is trying to pin down what exactly the patient means – is this Lightheaded, Pre-syncopal, Vertigo, or disequilibrium.
Vertigo is a false perception of rotation of the external world (objective vertigo) or of the individual in space (subjective vertigo)
Pre-syncope is a feeling of impending fainting/LOC
Disequilibrium is impaired balance and gait in the absence of an abnormal head sensation
Light-headedness is a non specific description that doesnt fit with one of the above.
Before we move on and focus in on vertigo and disequilibrium. People often feel Pre-syncopal (and will describe it as lightheaded) when their oxygen supply to their brain was reduced – most likely through a drop in their blood pressure. Think about the feeling you get when you stand up to quick - this temporary sensation is from poor brain perfusion due to the change in posture. The increase in height, and the need for increased pressure, has happened faster than the body’s reflexes can compensate (in this instance by increased HR). This is often exacerbated by relative hypovolaemia (being dehydrated as one example) or by medications that limit the ability of our heart to speed up (think about all the old people who have postural hypotension and how its exacerbated by their beta-blockers).
Understanding Balance and equilibrium
Equilibrium is a complex mechanism with many sensory inputs – Vestibular Apparatus, Visual input and then proprioception input from the neck and the rest of the body.
The vestibular apparatus feeds the vestibular nuclei in the brainstem via the vestiibulocochlear nerve. The apparatus consists of the membranous labyrinth contained within the bony labyrinth ring in the petrous temporal bone. The membranous labyrinth consists of 3 semicircular canals and 2 chambers (saccule and utricle). The flow of endolymph in the canals stimulates cilia attached to the sensory organ in the ampulla (crista ampullaris). In the saccule and urtricles the movement of calcium carbonate crystles stimulates the cilia of the macula. This means that there is modification of the neural impulses in all planes of head movement. Vertigo results from an imbalance or disconnect in any of the sensory inputs to the brainstem.
Nystagmus consists of an inital smooth movement in one direction folloed by a rapid movement (saccade) in the opposite. – the direct of the fast movement or beat is used to describe the nystagmus. When the fast component is left then it is leftbeat nystagmus. On far lateral gaze it can be normal.
Peter Johns is the go to guy for video explainers – here is his youtube channel https://youtube.com/@peterjohns?si=jT_nfzCZ24zJTLqm
Then, once we have established that the patient has vertigo (not one of the other descriptions of dizziness), we need to work out whether their vertigo is peripheral or central. The big 3 diagnoses we see are BPPV, Vestibular Neuritis and more rarely, but much more significantly, Posterior Circulation Stroke.
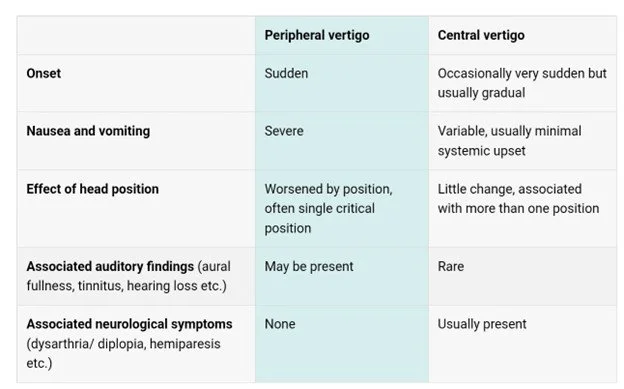
The history in these patients may be confusing and imprecise. This table from RCEM Learning gives us the clues of where the vertigo is coming from:
When Examining the patient we need to be considering all causes of vertigo and associated conditions – such as AF. A good general neurological exam will allow us to screen for associated neurological conditions such as CN 5 and 7 palsies and vertigo suggesting cerebellopontine tumours and Limb ataxia suggesting cerebellar disease.
An ear exam may show us Ramsey Hunt, (herpes zoster infection in the facial nerve) or evidence of a cholesteatoma or TM perforation.
Hearing should be assessed through the finger rub test and hearing loss and central vertigo is suggestive of an inferior, posterior circulation infarct.
The next test is an assessment of Nystagmus, a patient that doesnt have spontaneous nystagmus, that is nystagmus with a still head, does not have a central cause and the patient does not need a HINTS plus exam.
HINTS Plus exam- these signs can be interpretted as either peripheral or central (note some of the central features can be normal, which is why we refer to them as a peripheral or a central sign as opposed to positive/negative or normal/abnormal)
Head Impulse
· Line the patient up infront of you and hold on to each side of their head.
· Ask them to fix their gaze to your nose
· Rotate the head 20-40degrees to each direction and then rapidly bring it back central
In peripheral causes the vestibulo-ocular reflex is distrupted so the patient looses eye contact and then corrects wtih a saccade. A normal response if being able to maintain eye contact.
Nystagmus
· Peripheral Nystagmus is always horizontal with the fast phase in the same direction.
· Vertical or rotational Nystagmus is suggestive of a central cause
· Multidirectional Nystagmus is a strong sign of a central cause.
Test of Skew
· Stand the patient in front of you
· Ask the patient to fix their gaze to your nose
· Alternatively cover their eyes
In Central Vertigo the vertical alignment of the eyes maybe different and a vertical movement will be seen when the eye is covered and uncovered.
The Plus part of HINTS Plus – is a finger rub test of hearing. Most causes of hearing loss and vertigo are peripheral but this isnt a one size fits all, as inferior posterior circulation stroke can take out hearing as well as cause vertigo – these patients will also have other signs of central vertigo.
A really good gross neurological examination is can the patient stand and walk? Even those with really bad BPPV or Vestibular Neuritis will be able to walk, admittedly it maybe slow and difficult but they will be able to. Being unable to walk is a good sign for posterior circulation stroke.
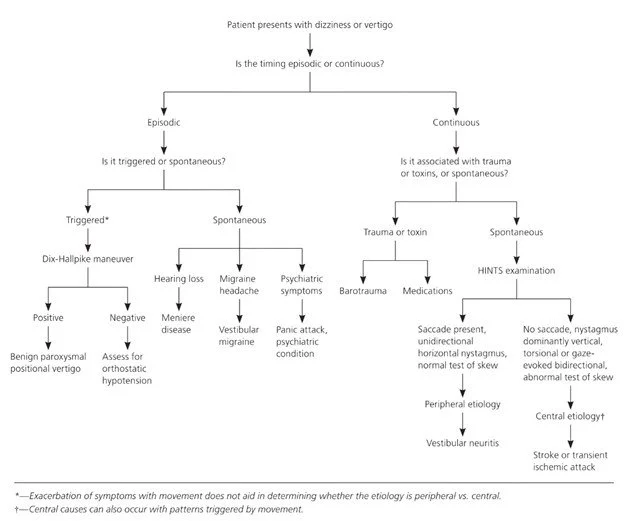
This flow diagram summarises the thought process nicely.
Causes of Vertigo:
We cant always find a cause of a patient’s vertgio. The safest way to think about it is to rule out significant pathology that isnt self limiting. That is “could this be a posterior circulation stroke?”. Then its about symptom control – a diagnosis help prognosticate and reduces the chance of us missing something.
First the Peripheral Causes.
Acute Vestibular Neuritis
Typically caused by a viral infection leading to inflammation of the vestibular nerve. Commonly seen in young/middle aged adults and is the most common cause of prolonged peripheral vertigo.
· Acute Onset within minutes/hours
· Exacerbated by head movements
· Often severe nausea or vomiting
· No other neurological deficit
· No hearing loss
· 2/3s have spontaneous nystagmus
o Horizontal
o Unidirectional
o Suppressed by visual fixation
o Fast phase away from affected ear and most evident when looking to unaffected side.
Over a few days patients begin to improve as their vestibular system starts to compensate. In 50% of patients the nerve damage may take 2 months to resolve leaving the patient with a sense of disequilibrium and recurring vertigo. These episodes should become shorter with time and if they dont another diagnosis should be considered. Interestingly 15% of patients with Vestibular Neuritis may develop BPPV after.
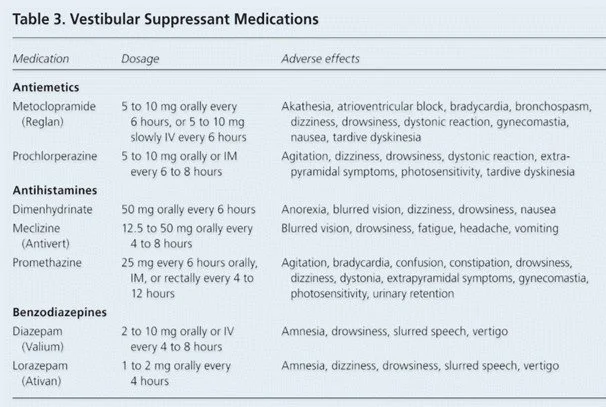
Treatment is Vestibular Suppression and antiemetics
My preferred drug is prochlorperazine, its effective and covers both antiemetic effects and suppresses the vestibular system. Vestibular Suppressants should only be used for 3 days as they interfere with the normal compensatory mechanisms, leading to an increased falls risk.
Benign Positional Paroxysmal Vertigo (BPPV)
A very common condition caused by dislocation of the otoconia (canalitihs) into the semi-circular canals, most commonly the posterior canal. Often there is no trigger but has been associated with head trauma in younger people. Vertigo is related to changes in head position and tends to be short lasting and intermittent.
It is diagnosed with the Dix-hallpike test and treated with the Epley Manoeuvre
https://youtu.be/kvVnEsGVLUY?si=gVtZWNPT4_v2TNA0
Where possible avoid the use of pharmacological treatments – these may suppress compensatory mechanisms and increase the risk of falls. The real treatment needed in the Epley Manoeuver.
Meniere’s Disease
Occurs at any age, although typically between 20 and 60. Presents with vertigo and unilateral hearing loss. There may be associated headache. Unidirectional, horizontal -rotational nystagmus when the patient has vertigo
Pathology: Excess endolymphatic fluid pressure leading to inner ear dysfunction.
It is initially treated with Prochlorperazine or an antihistamine like cyclizine.
It is a long term condition that may benefit from ENT/physio input.
Typically the vertigo is debilitating but an acute attack only lasts 24hrs. Betahistine can be used as prophylaxis.
Central Causes:
Cerebellar Stroke
This is the diagnosis everyone worries about missing, it is hugely debilitating and potentially treatable or ‘rehab-able’. These patients are typically old and have cardiovascular risk factors when compared to those with Vestibular Neuritis. As its a vascular problem, onset is hyperacute, immediate, within a few seconds.
The vertigo is unaffected by head position, with little nausea and often with co-existing neurological deficits (the characteristics of a central vertigo)
The nystagmus can be horizontal, rotatory or vertical. Its bidirectional and not suppressed by visual fixation.
Watch this video by Peter John to clarify the nystagmus in the Big 3 causes of vertigo https://youtu.be/MwbqJvMDonU?si=3_2X-wGSn2-zV-tv
Vestibular Migraine
Migraine like headaches with vertigo that maybe either peripheral or central in nature – please have a look at the headache section for more on migraines.
Treatments
Beyond the treatment of the underlying cause, vestibular suppressants listed above and management of dehydration and the inability to take oral medications patients may need vestibular exercises to aid their compensatory mechanisms and reduce function loss. Examples of these exercises (for acute peripheral vertigo):
1. Maintain focus on an object, move head from side to side and up and down. Start slowly and with small movements and gradually increase speed and amplitude. Repeat 2-3 times a day
2. An alternative can be keeping the head still and just moving the eyes.